Improving Outcomes for Clinical Surgery Patients
Our research addresses the full spectrum of evidence-based surgical practice including
- Surgical clinical trials
- Cost-effectiveness studies of new surgical interventions
- Systematic reviews of the literature and meta-analysis
- Studies of the actual uptake of research evidence and clinical practice guidelines into surgical practice
- Measurement of patient preferences for alternate treatment options
- Long-term studies of patient outcomes following surgical procedures.
SOuRCe undertakes a broad range of clinical and health service research that aims to improve outcomes for surgical patients. All projects follow a multidisciplinary approach bringing together expertise in clinical science, epidemiology, health economics and health psychology. Projects frequently include students and trainee clinicians to provide research training opportunities.
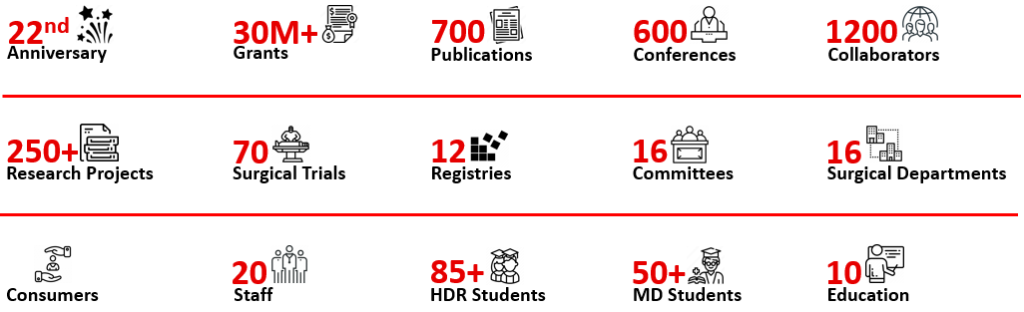
Our Overall Research Output
Currently, SOuRCe is involved in over 250 research studies in collaboration with multi-specialty surgical departments, allied health, nursing, other academics and consumers, based in Australia and Internationally. Over 55% of our research studies are registry-nested and originate from comprehensive data collected from the funded surgical programs, including the Advanced Gastrointestinal Research Program, Robotics Program, Orthopaedic Surgery and Vascular Surgery Programs. The other 45% of our research originates from historical collaborations within the following departments: colorectal, transplant, urology, ear, nose and throat, orthopaedics, upper gastrointestinal, breast, vascular, allied health, head and neck, anaesthetics, nursing, benign gynaecology, pathology, imaging, pharmacy and other departments and institutions.
Over the past 22 years, SOuRCe has rapidly developed to become one of the major Australian surgical research units, and is now a centre of surgical research excellence with international recognition. During this time, SOuRCe was awarded over $30M in competitive funding, including major funding bodies such as the NHMRC, MRFF, CINSW, NIHR and others. SOuRCe has published over 700 peer-reviewed scientific articles in the top surgical and medical journals, including NATURE, BMJ, JAMA surgery, Annals of Surgery, The British Journal of Surgery, Journal of Surgical Oncology and others high impact journals. SOuRCe has supervised over 85 PhD and MPhil students and over 50 MD students. These achievements have contributed significantly to the enhancement of patient outcomes and have changed clinical practice at RPAH, Australia and Internationally.
Funded Research Programs
Our funded surgical research programs include the Advanced Gastrointestinal Surgical Program (including Pelvic Exenteration, Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy, Retroperitoneal Sarcoma and Advanced Upper Gastrointestinal Surgery), Robotics Program, Orthopaedic Surgery, Vascular Surgery, and the Preoperative Optimisation Research Program. Most of the funded research programs are governed by the RPA Institute of Academic Surgery and are led by a large amount of multidisciplinary and multispecialty groups of clinical and non-clinical staff from a variety of departments across RPAH.
- Pelvic Exenteration Research Program
- Upper Gastrointestinal Surgery Research Program
- Peritoneal Malignancy Research Program
- Orthopaedic Surgery Research Program
- Retroperitoneal Sarcoma Research Program
- Preoperative Optimisation Research Program
- Robotic Surgery Research Program
- Bone and Soft Tissue Sarcoma Research Program